Abstract
Introduction: The majority of acute lymphoblastic leukemia (ALL) deaths occur in adults, with only 40% of adult ALL patients achieving 5-year leukemic-free survival, and decreasing cure rates with increasing age (Abuasab 2021). ALL treatment is variable across facilities, based on patient and disease features, along with institutional factors (Khullar, 2022). Currently, there are limited studies that investigate adult ALL overall survival (OS) outcomes by facility characteristics. The primary objective of our study was to determine adult ALL OS by facility volume and type for adult patients.
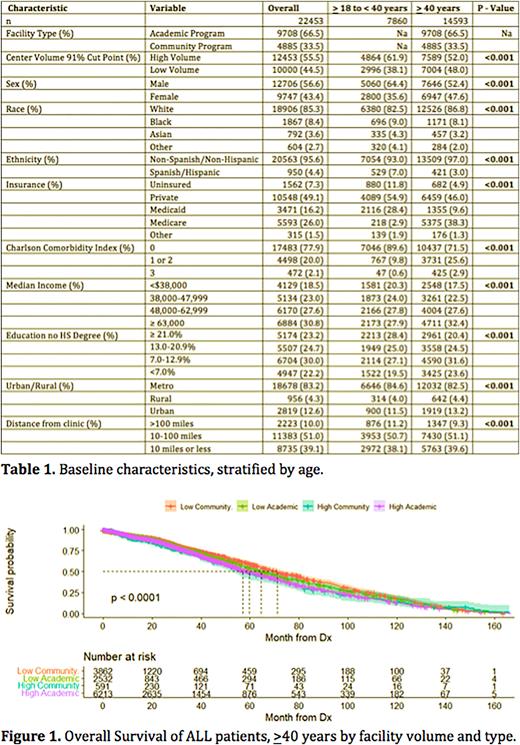
Methods: This retrospective study analyzed de-identified National Cancer Database (NCDB) files from 2004-2016. ALL patients >18 years of age met inclusion criteria. Facility type was not available for patients <40 years of age, and was excluded from analysis. Baseline patient characteristics were extracted and sub-grouped by age >18 to <40 and >40. Summary statistics included frequency (%) for categorical variables and median [IQR] for non-normal continuous variables. Group differences were compared with Chi-square or Kruskal-Wallis rank sum tests. Facility volume was determined by a maximally selected log-rank statistics, with high volume (HV) versus low volume (LV) cut point at >91%. Academic programs (APs) included academic/research and integrated network cancer programs. Community programs (CPs) included community and comprehensive community programs. OS Kaplan Meier (KM) curves censored by death or last follow-upwere created for facility volume and type. Analysis was conducted with R software 4.0.3. The NCDB is a joint project of the Commission on Cancer of the American College of Surgeons and the American Cancer Society, these institutions have not verified and are not responsible for the methodology or findings of this research.
Results: 22,453 ALL patients were included in the study (>18 to <40 years N=7860; >40 years N=14,593). 12,453 (55.5%) patients were treated at HV and 10,000 (44.5%) at LV centers. 9708 (66.5%) of patients >40 years were treated at APs and 4885 (33.5%) patients were treated at CPs. For both age cohorts, patients were more likely to be male, White, Non-Hispanic, have a Charlson Comorbidity Index of 0, private insurance, a median income >$63,000, and reside in a metro area 10-100 miles from the treatment center (P < 0.001)(Table 1). Analysis of patients >18 to <40 years found no significant OS difference between patients treated at LV and HV centers (mOS 64.4 mo., 95% CI 62.2-67.6 vs. 60.9 mo., 58.2-63.4; p = 0.1). Analysis of patients >40 years found longer OS in patients treated at LV CP (red line) compared to HV AP (purple line) (mOS 71.1 mo., 95% CI 66.6-75.8% vs. mOS 56.9 mo., 95% CI 56.6-62.7; P <0.0001) (Figure 1). OS was greater at LV compared to HV centers (mOS 68.7 mo., 95% CI 65.2-71.5 vs. 59.5 mo., 95% CI 56.6-62.3; P < 0.0001) and OS was greater at CPs compared to APs (mOS 69.2 mo., 95% CI 65.0-72.6 vs. 61.2 mo., 95% CI 58.5-63.4; p = 0.00049).
Discussion: This large, national study provides insight into OS in adult ALL patients by treatment facility. Despite a paucity of differences in patient characteristic trends between age cohorts, we found OS differed by facility volume in older ALL patients but not younger adult patients. Interestingly, OS of young adult ALL patients was not uniformly superior to older patients. OS in patients >40 years was longest in those treated at LV and CPs, and shortest amongst patients treated at HV and APs. Potentially, patients with more advanced/high-risk disease, and therefore worse prognosis, were selectively treated at HV and APs, accounting for inferior OS. Additionally, perhaps more aggressive treatments were attempted at HV and APs, increasing risk of death in the older adult population. Finally, differences in sociodemographics may have driven OS differences. Our study was limited by its retrospective nature, the delay in reported NCDB data and current clinical practice, and missing facility type for patients <40 years.
Conclusion: OS in adult ALL patients >40 years was significantly different by facility volume and type, with the greatest OS in patients treated at LV and CPs, and the least OS at HV and APs. Amongst patients >18 to 40 years of age, there was no difference in OS by facility volume. Future research is needed to understand and improve adult ALL OS trends observed between treatment facilities.
Disclosures
Lai:Astellas, Jazz: Speakers Bureau; AbbVie, Agios/Servier, Daiichi-Sankyo, Jazz, Macrogenics, PDS, Pfizer, Genentech, Taiho, Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal